Septic Shock: Diagnosis & Management for USMLE Success | Integrated USMLE Prep
Why septic shock is always on exams
Septic shock is a Step‑2 favorite because it blends infectious disease, cardiovascular physiology, and critical care. It’s deadly in real life and tricky on tests because they want you to spot hypotension from sepsis vs hemorrhage vs cardiogenic causes and respond with the right fluids, antibiotics, and pressors.
Step 1 integration: Endotoxin (LPS) binds TLR‑4 on macrophages → release of TNF‑α, IL‑1, and IL‑6 → nitric oxide‑mediated vasodilation and ↑ vascular permeability → distributive shock physiology.
Stepwise definitions (updated Sepsis‑3)
- SIRS (Systemic Inflammatory Response Syndrome): 2+ of temp abnormal, tachycardia, tachypnea, leukocytosis/leukopenia.
- Sepsis: Life‑threatening organ dysfunction due to dysregulated host response to infection.
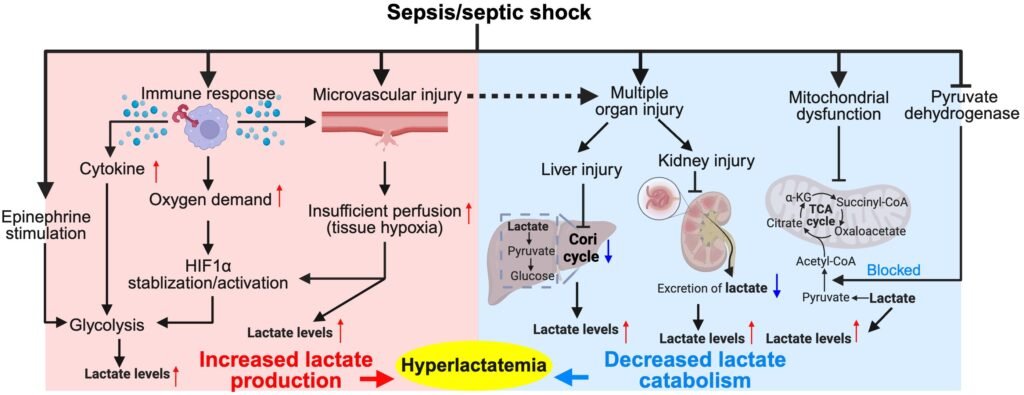
- Septic shock: Sepsis + hypotension requiring vasopressors to maintain MAP ≥65 mmHg and lactate >2 mmol/L despite adequate fluids.
Step 1 integration: Lactate elevation reflects anaerobic metabolism from poor tissue perfusion.
Clinical vignette #1 — elderly pneumonia patient
A 72‑year‑old man with fever, productive cough, and confusion. Vitals: BP 78/40, HR 125, RR 28, O₂ sat 89% on RA. Labs: WBC 19k, lactate 5 mmol/L.
Moves:
- Blood cultures.
- Broad‑spectrum antibiotics (within 1 hour!).
- 30 mL/kg IV crystalloid bolus.
- Norepinephrine if hypotension persists.
Step 1 integration: Norepinephrine is an α₁ agonist → vasoconstriction raises systemic vascular resistance; β₁ effect helps cardiac output.
Clinical vignette #2 — post‑op abdominal catastrophe
A 58‑year‑old woman post‑colectomy has abdominal distension, fever, hypotension (BP 70/40), tachycardia, and rising creatinine.
Diagnosis: septic shock from intra‑abdominal abscess/leak.
Moves:
- IV fluids + pressors.
- Broad‑spectrum antibiotics (cover gram‑negatives + anaerobes).
- Source control: urgent return to OR for washout.
Step 1 integration: Persistent infection maintains cytokine storm → endothelial dysfunction → capillary leak → third‑spacing of fluids → distributive shock.
Pathophysiology in plain English
- Distributive shock: systemic vasodilation → low SVR, warm extremities, bounding pulses.
- Capillary leak: albumin and plasma leak into interstitial space → edema, ↓ preload.
- Mitochondrial dysfunction: even if perfusion restored, cells struggle with oxygen utilization.
- Cardiac depression: TNF‑α and IL‑1 blunt contractility.
Step 1 integration: Endotoxin triggers NO synthase upregulation → cGMP‑mediated smooth muscle relaxation → refractory hypotension.
Workup & labs
- CBC: leukocytosis or leukopenia.
- Lactate: marker of hypoperfusion.
- Blood cultures (before antibiotics).
- Source‑specific imaging (CXR, CT abdomen).
Management framework (memorize this order)
- Airway & oxygen as needed.
- Early IV fluids: 30 mL/kg crystalloids within first 3 hours.
- Antibiotics within 1 hour after cultures.
- Vasopressors: norepinephrine first‑line; add vasopressin or epinephrine if refractory.
- Source control: drain abscess, remove infected catheter, surgery if needed.
- Adjuncts: stress‑dose steroids if pressor‑refractory and concern for adrenal insufficiency.
Step 1 integration: Vasopressin is a V1 agonist → vascular smooth muscle constriction via IP₃/Ca²⁺ signaling.
Exam pearls
- Don’t give dopamine (arrhythmogenic, worse mortality).
- Warm extremities = distributive shock (vs cold in hypovolemic/cardiogenic).
- Never delay antibiotics for imaging.
- Procalcitonin can help distinguish bacterial sepsis vs noninfectious inflammation.
- ScvO₂ <70% suggests inadequate tissue oxygen delivery.
Quick table: Differentiating shock types
| Shock type | SVR | CO | Extremities |
|---|---|---|---|
| Hypovolemic | ↑↑ | ↓↓ | Cold/clammy |
| Cardiogenic | ↑↑ | ↓↓ | Cold/clammy |
| Distributive | ↓↓ | ↑ or ↓ | Warm, flushed |
Complications of septic shock
- Acute kidney injury (ischemia).
- ARDS (capillary leak in lungs).
- DIC (endothelial injury + tissue factor release).
- Multi‑organ dysfunction.
Step 1 integration: TNF‑α and IL‑1 induce tissue factor expression on endothelium → coagulation cascade activation → microthrombi → consumptive coagulopathy.
Take‑home summary
Septic shock = sepsis + hypotension + high lactate despite fluids.
Treat with rapid fluids, antibiotics, norepinephrine, and source control.
On exams, always pick antibiotics within 1 hour and 30 mL/kg fluids as first moves.
Step 1 recap: LPS → cytokine storm → NO vasodilation → distributive shock. Lactate is the biomarker. Norepinephrine is the pressor of choice.
Thanks again for stopping by! Be sure to check out our other blogs or contact us for tutoring today!