Pulmonary Embolism: Rapid Diagnosis and Management Guide | Integrated USMLE Prep
Why this matters
Pulmonary embolism (PE) is a fast‑moving killer that rewards a disciplined algorithm. This post gives you a bedside‑ready approach that matches exam logic and real‑world flow.
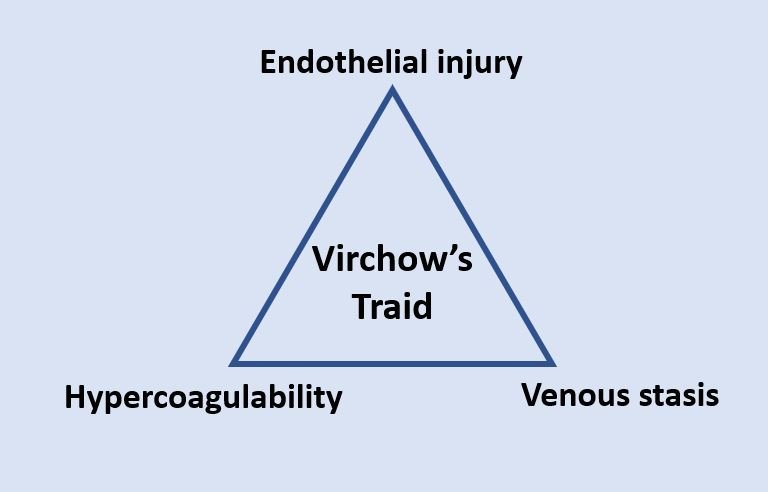
Step 1 integration: Virchow triad—stasis, endothelial injury, hypercoagulability—frames DVT/PE risk. Factor V Leiden (APC resistance) and antithrombin deficiency are classic test fodder.
USMLE/Step 2 CK 30‑Second Algorithm for diagnosis of pulmonary embolism
1) Pretest probability → Wells or clinical gestalt.
2) Low risk → apply PERC; if negative, no testing.
3) Fails PERC or intermediate risk → D‑dimer. If positive → imaging.
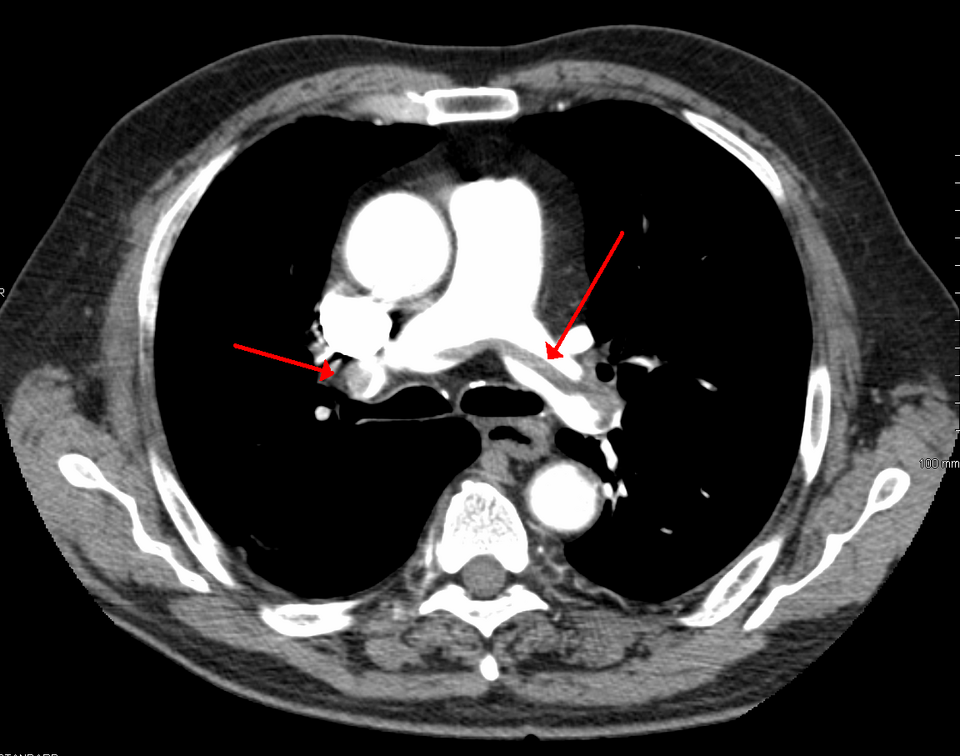
4) High risk/unstable → CTPA (or bedside echo if crashing); start anticoagulation unless contraindicated.
5) Massive/submassive → consider systemic thrombolysis or catheter‑directed therapy; evaluate for thrombectomy in select cases.
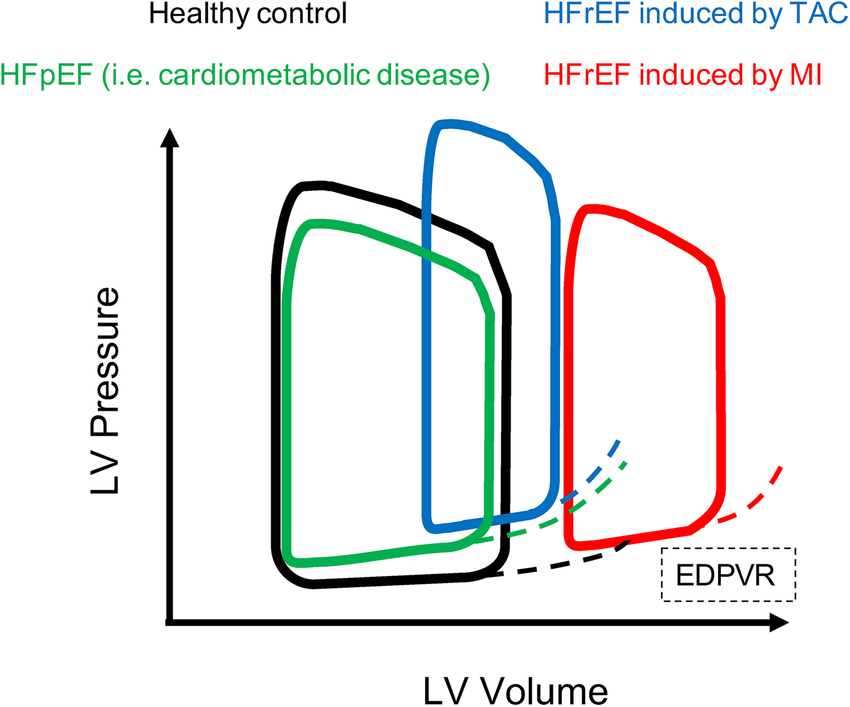
Step 1 integration: V/Q mismatch in PE = increased dead space, ↓ETCO₂, hypoxemia from shunt‑like areas and impaired diffusion reserve.
PE Risk Tools You’ll Actually Use
Wells score (key items):
- Signs of DVT (3), PE most likely (3), tachycardia (1.5), immobilization/surgery (1.5), prior VTE (1.5), hemoptysis (1), malignancy (1).
- Low (≤4), Intermediate (4.5–6), High (≥6.5) in many schemas.
PERC (rule‑out in low risk only): age <50, HR <100, O₂ sat ≥95%, no hemoptysis, no estrogen, no prior VTE, no unilateral leg swelling, no recent surgery/trauma.
Step 1 integration: D‑dimer = fibrin degradation product; high sensitivity, low specificity—great to rule out when pretest probability is low.
PE Imaging Strategy
- CT pulmonary angiography (CTPA): first‑line in most; shows filling defects, RV strain.
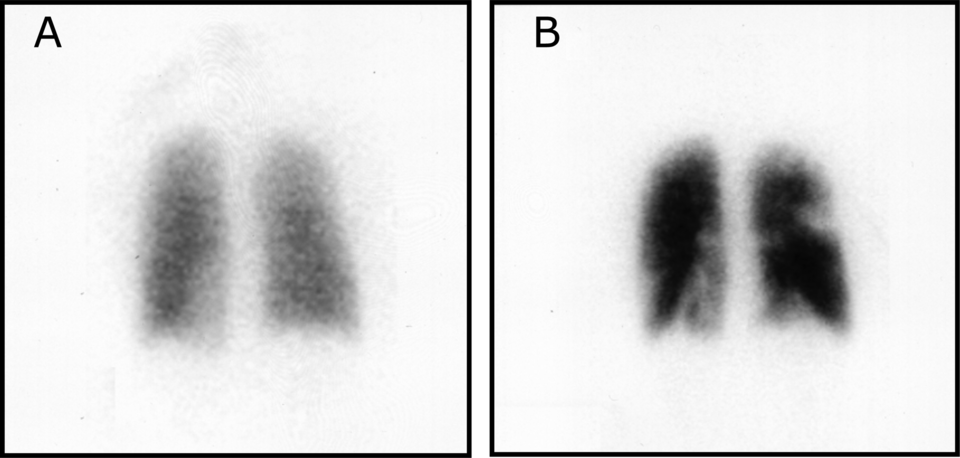
- V/Q scan: preferred in pregnancy, contrast allergy, or renal impairment; look for segmental perfusion defects with preserved ventilation.
- Bedside echo in shock: RV dilation, septal flattening (D‑sign) → supports massive PE.
Step 1 integration: West zones & gravity: perfusion drops apically; PE exaggerates regional V/Q, creating zones with high V/Q (dead space).
PE Initial Management (don’t wait on a perfect scan if crashing)
- Anticoagulation unless contraindicated:
- Heparin (UFH) if potential for procedures/lysis or renal failure.
- LMWH/DOACs (apixaban, rivaroxaban) for most stable patients.
- Oxygen, hemodynamic support; avoid excessive fluids in RV failure; consider norepinephrine if hypotensive.
Step 1 integration: Heparin activates antithrombin III → inhibits IIa/Xa; protamine reverses UFH. DOACs inhibit Xa (rivaroxaban, apixaban) or IIa (dabigatran).
Reperfusion & Advanced Options
- Massive PE (hypotension): systemic thrombolysis (alteplase) if no absolute contraindications.
- Submassive PE (RV strain, normal BP): consider catheter‑directed lysis or mechanical thrombectomy in select patients.
- IVC filter only if absolute contraindication to anticoagulation or recurrent PE despite adequate therapy.
Step 1 integration: Thrombolytics = plasminogen → plasmin activation (fibrinolysis). Absolute CI: prior intracranial hemorrhage, known AVM, ischemic stroke <3 mo (except recent small), etc.
Risk Stratification & Disposition
- Use PESI/sPESI, troponin/BNP, and RV strain on imaging to guide admission vs early discharge.
- Cancer‑associated VTE: LMWH or DOACs; watch GI/GU bleed risk.
Step 1 integration: S1Q3T3 on ECG is classic but insensitive; ABG often shows acute respiratory alkalosis (hyperventilation) with widened A–a gradient.
Special Populations and Pulmonary embolism
- Pregnancy: start heparin (UFH/LMWH); avoid warfarin. Prefer V/Q if CXR normal; CTPA reasonable if CXR abnormal.
- Severe CKD/contrast allergy: V/Q favored.
- Recent surgery/ICH: weigh risk; consult for catheter therapy.
Pitfalls (high‑yield)
- Ordering D‑dimer in high‑risk patients (wastes time).
- Over‑resuscitating RV failure with liters of fluid.
- Missing post‑partum VTE risk or estrogen exposure.
- Stopping anticoagulation too early in provoked vs unprovoked VTE—plan 3 months minimum for provoked; consider extended therapy if unprovoked/ongoing risk.
Micro‑vignettes
- Post‑op day 3, tachy + pleuritic CP, Wells high → start UFH, get CTPA; consider lysis if hypotensive.
- Low‑risk URI patient, meets all PERC → no testing.
- Pregnant with pleuritic CP, normal CXR → V/Q scan; treat with LMWH if positive.
Thanks again for stopping by! Be sure to check out our other blogs or contact us for tutoring today!
Keywords: pulmonary embolism, Wells score, PERC rule, D‑dimer, CTPA, V/Q scan, thrombolysis, catheter‑directed therapy, RV strain, PESI, USMLE Step 2