Hyponatremia for Step 2 | Integrated USMLE Prep
Keywords: hyponatremia, SIADH, urine osmolality, urine sodium, hypotonic hyponatremia, osmotic demyelination, DDAVP clamp, USMLE Step 2
Why this matters
Hyponatremia is common, sneaky, and dangerous when corrected incorrectly. This guide gives you a rapid, exam‑proof approach you can run at 3 a.m. without breaking a sweat.
Step 1 integration: Osmolality drives water shifts. ADH modifies collecting duct water permeability via V2→Gs→cAMP→AQP2 insertion.
10‑Second Algorithm (then details)
- Confirm true hypotonic hyponatremia.
- Assess severity & symptoms. Seizure/coma? Give 3% saline bolus.
- Classify by volume status: hypo‑ / eu‑ / hypervolemic.
- Use urine Osm and urine Na to pinpoint cause.
- Treat cause and correct slowly (limits below).
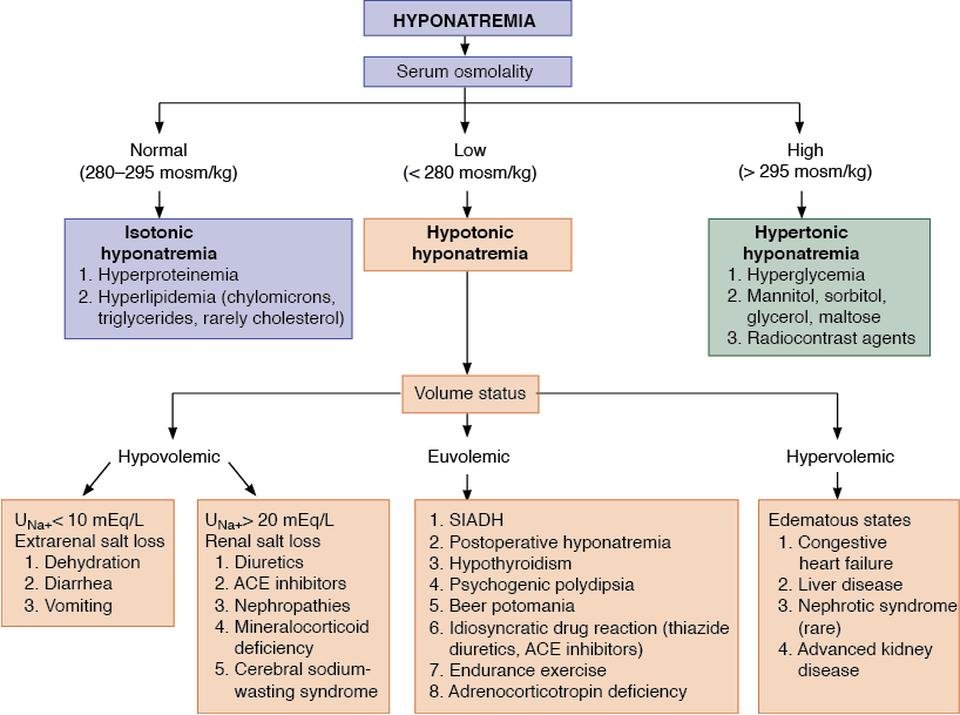
First: Confirm it’s hypotonic hyponatremia
- Serum Osm:
- >295 → hypertonic (e.g., hyperglycemia).
- 275–295 → isotonic (pseudohyponatremia: severe hyperlipidemia/proteinemia).
- <275 → true hypotonic (proceed).
Step 1 integration: Corrected Na in hyperglycemia ≈ Nacorr = Nameas + 1.6 × [(Glucose − 100)/100] (classic exam value).
Second: Severity & emergency treatment
Red flags: seizures, obtundation, respiratory arrest, signs of impending herniation.
- Give 3% saline 100 mL IV bolus over 10 minutes; may repeat up to 3 times for ongoing severe symptoms.
- Target initial rise ≈4–6 mEq/L to stop seizures.
Step 1 integration: Rapid brain adaptation to chronic hyponatremia (loss of organic osmolytes) explains risk for osmotic demyelination with overcorrection.
Third: Classify by volume status
| Volume | Typical causes | Urine Osm | Urine Na |
|---|---|---|---|
| Hypovolemic | GI losses, thiazides, mineralocorticoid deficiency | >100 | >20 (renal losses) or <20 (extrarenal) |
| Euvolemic | SIADH, hypothyroid, adrenal insuff., primary polydipsia/low‑solute diet | SIADH >100; polydipsia/low solute <100 | SIADH >30 |
| Hypervolemic | Heart failure, cirrhosis, nephrotic syndrome | >100 | usually <20 (unless on diuretics) |
Step 1 integration: SIADH = inappropriately high ADH → concentrated urine (high Osm), natriuresis (↑urine Na), low serum uric acid.
Fourth: Etiology clues from urine studies
- Urine Osm <100 mOsm/kg → excess water intake or low solute (primary polydipsia, beer potomania).
- Urine Osm >100 + Urine Na >30 → SIADH, renal salt wasting, adrenal insufficiency, hypothyroidism.
- Urine Osm >100 + Urine Na <20 → effective arterial volume depletion (HF, cirrhosis).
Fifth: Treatment playbook
Hypovolemic hypotonic hyponatremia
- Isotonic saline (0.9%) to restore volume → suppresses ADH → Na rises.
- Stop offending diuretics; consider mineralocorticoid replacement if adrenal cause.
Euvolemic (SIADH)
- Fluid restriction (e.g., ≤800–1000 mL/day).
- Increase solute: salt tabs + loop diuretic or urea.
- Vaptans (tolvaptan) for refractory cases (avoid in severe symptoms—use 3%).
- Treat underlying cause (pain, nausea, pulmonary/CNS disease, meds: SSRIs, carbamazepine).
Hypervolemic
- Fluid + sodium restriction, loops, optimize HF/cirrhosis/nephrotic management.
- Consider vaptans in select hospitalized patients.
Correction limits (don’t cause ODS)
- Chronic hyponatremia: aim ≤8 mEq/L in 24 h (many target 4–6).
- High ODS risk (Na ≤105, alcoholism, malnutrition, liver disease, hypokalemia): aim ≤4–6 mEq/L/24 h.
- If Na is rising too fast: DDAVP clamp + D5W to re‑lower safely.
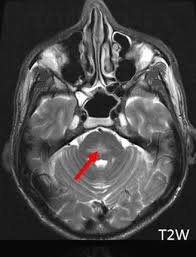
Step 1 integration: ODS (classically central pontine myelinolysis) → acute quadriparesis, dysarthria, “locked‑in” signs. Prevent by slow correction.
Practical calculations you actually use
- Sodium deficit (mEq) ≈ (Nagoal − Naactual) × TBW
TBW ≈ 0.6 × weight(kg) men, 0.5 women; elderly often less. - 3% saline contains ≈513 mEq/L Na (~0.513 mEq/mL).
- Expected ΔNa with 3% bolus (100 mL) ≈ 0.5–1.5 mEq/L depending on size/TBW.
Step 1 integration: Edelman equation conceptually links serum Na to exchangeable Na+K over TBW—why both water and potassium shifts matter.
Common pitfalls (high‑yield)
- Normal saline in SIADH can worsen Na (desalination) when urine Osm > infused Osm.
- Treat adrenal insufficiency (give steroids) before fluid alone.
- Always check TSH, AM cortisol, meds, and uric acid in unexplained euvolemia.
- Don’t forget hypokalemia—correcting K+ raises serum Na.
Mini‑vignettes (exam style)
1) Marathoner + diarrhea, Na 122, U Osm 450, U Na 10 → Hypovolemic: NS resuscitation.
2) Post‑op on SSRIs, Na 118, U Osm 600, U Na 45, euvolemic → SIADH: fluid restrict, consider salt + loop.
3) Schizophrenia, Na 124, U Osm 60 → Primary polydipsia: water restriction, ↑dietary solute.
Thanks again for stopping by! Be sure to check out our other blogs or contact us for tutoring today!

