Acute Coronary Syndromes: Mastering the USMLE Step 1 and Step 2 Integration
Keywords: acute coronary syndrome USMLE, ACS Step 1 Step 2, STEMI NSTEMI pathophysiology, coronary artery disease medical student, cardiology shelf exam prep
Acute coronary syndromes (ACS), and cardiology in general, represent one of the highest-yield topics across all USMLE examinations and clinical rotations. The beauty of ACS lies in its perfect integration of basic science foundations with clinical decision-making—exactly what the new Step 2 format emphasizes. This comprehensive guide will help you master ACS by connecting pathophysiology, pharmacology, and clinical management in a way that prepares you for success on both standardized exams and the wards.
Understanding the ACS Spectrum: From Pathophysiology to Bedside
Acute coronary syndrome encompasses three distinct but related conditions: unstable angina (UA), non-ST-elevation myocardial infarction (NSTEMI), and ST-elevation myocardial infarction (STEMI). The key to mastering ACS is understanding that these represent a continuum of coronary artery occlusion severity.
Step 1 Integration: The pathophysiologic basis of ACS begins with atherosclerotic plaque rupture or erosion. Vulnerable plaques contain a large lipid core with a thin fibrous cap rich in inflammatory cells (macrophages, T-lymphocytes). When the cap ruptures, tissue factor is exposed, initiating the extrinsic coagulation cascade via factor VIIa, ultimately leading to thrombin generation and platelet aggregation.
Unstable Angina: The Warning Sign
Unstable angina represents acute coronary insufficiency without myocardial necrosis. Patients typically present with new-onset severe angina, rest angina, or crescendo angina (increasing frequency, severity, or duration of previously stable symptoms).
The pathophysiology involves partial coronary occlusion, usually due to non-occlusive thrombus formation over a ruptured plaque. Importantly, there’s insufficient coronary flow reduction to cause myocardial cell death, which is why cardiac biomarkers remain normal.
Step 1 Integration: Myocardial oxygen demand exceeds supply, but cellular ATP depletion hasn’t progressed to the point of membrane disruption and troponin release. The ischemia remains reversible, with anaerobic glycolysis temporarily maintaining cellular viability.
NSTEMI: Partial Occlusion with Necrosis
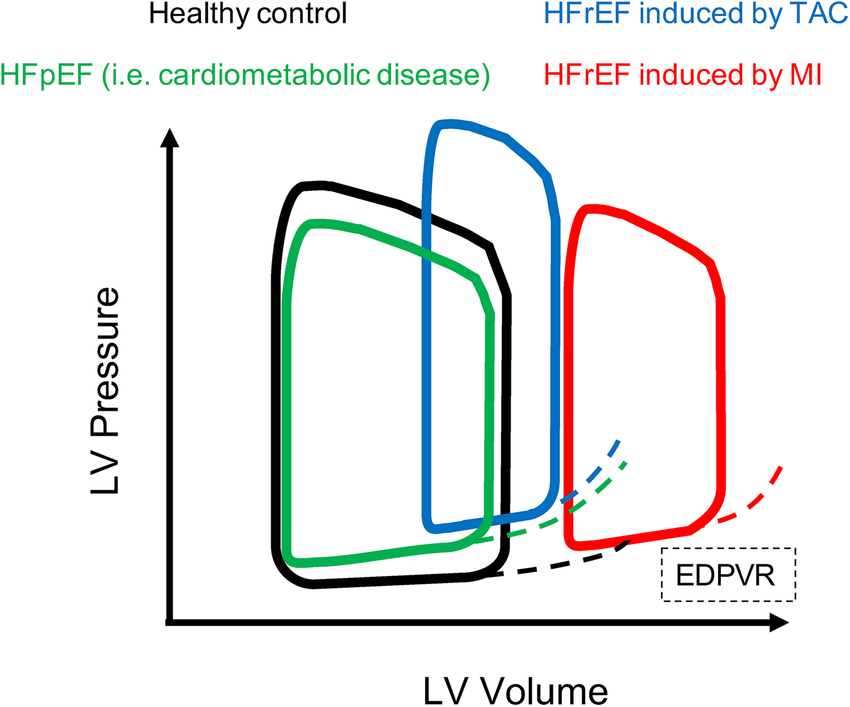
NSTEMI occurs when coronary occlusion is severe enough to cause myocardial cell death but doesn’t completely occlude the vessel or lacks sufficient collateral flow compromise to produce transmural infarction. This results in subendocardial necrosis—the area most susceptible to ischemia due to higher oxygen demand and lower perfusion pressure.
Step 1 Integration: The subendocardium is most vulnerable because it experiences the highest wall tension (Laplace’s law: tension = pressure × radius / 2 × wall thickness) and receives perfusion primarily during diastole when coronary perfusion pressure is lowest. When ATP is depleted, the Na+/K+-ATPase pump fails, leading to cellular swelling, membrane disruption, and troponin release.
STEMI: Complete Occlusion and Transmural Death
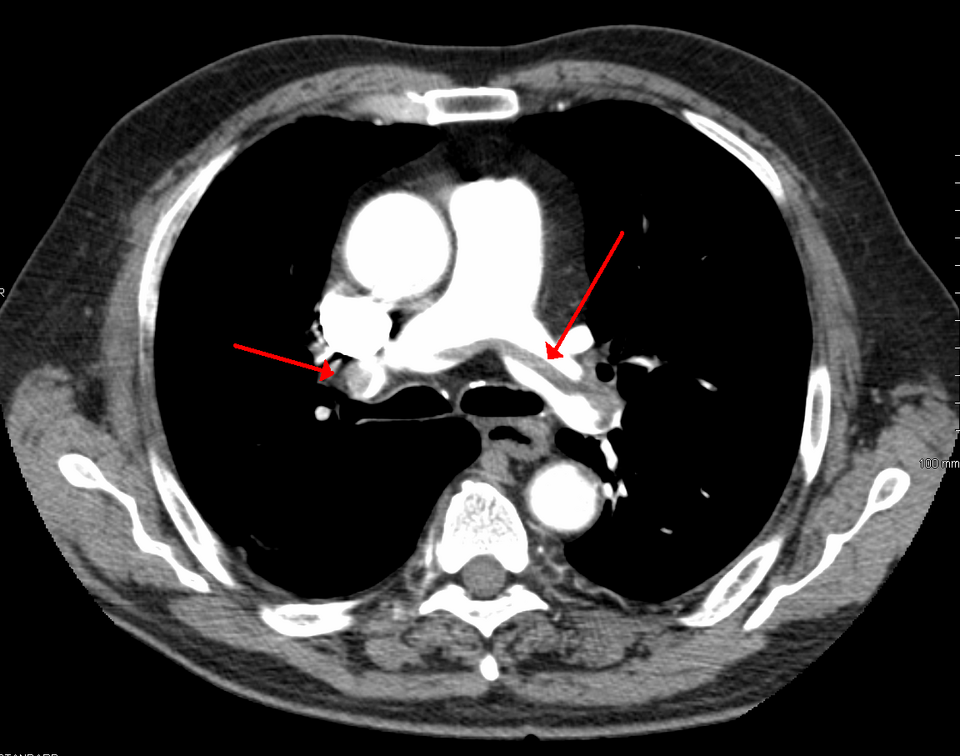
STEMI represents complete coronary artery occlusion leading to transmural myocardial infarction. The characteristic ST-elevation on ECG reflects the electrical injury pattern of transmural ischemia.
Step 1 Integration: Complete vessel occlusion creates a “current of injury” as the ischemic myocardium becomes electrically negative relative to normal tissue. This creates ST-segment elevation in leads facing the injured tissue and reciprocal ST-depression in opposite leads. The QRS changes (Q-waves) develop later as necrotic tissue becomes electrically silent.
Diagnostic Approach: Integrating Clinical Presentation with Laboratory and ECG Findings
Clinical Presentation Patterns
ACS typically presents with chest pain, but the character can vary significantly. Classic presentation includes substernal chest pressure with radiation to the left arm, jaw, or back, associated with diaphoresis, nausea, and dyspnea. However, atypical presentations are common, especially in women, elderly patients, and diabetics.
Step 1 Integration: Diabetic patients often have atypical presentations due to autonomic neuropathy affecting visceral pain sensation. The vagus nerve carries afferent fibers from the heart, and diabetic autonomic dysfunction can blunt the typical pain response.
Cardiac Biomarkers: Understanding the Molecular Basis
Troponin I and T are the preferred biomarkers for diagnosing myocardial infarction. These regulatory proteins control actin-myosin interaction in cardiac muscle and are released when myocyte membranes are compromised.
Step 1 Integration: Troponins are part of the thin filament regulatory complex along with tropomyosin. When intracellular calcium binds to troponin C, it causes a conformational change that moves tropomyosin, exposing myosin-binding sites on actin. Troponin release indicates irreversible membrane damage and correlates with the extent of myocardial necrosis.
High-sensitivity troponin assays can detect smaller amounts of myocardial necrosis earlier, but require careful interpretation of the kinetics. Troponin levels typically rise within 3-4 hours, peak at 12-24 hours, and remain elevated for 7-14 days.
ECG Interpretation in ACS
ECG changes in ACS follow predictable patterns based on the coronary anatomy and extent of occlusion:
- Anterior STEMI: ST-elevation in V1-V6 (LAD territory)
- Inferior STEMI: ST-elevation in II, III, aVF (RCA or LCX territory)
- Lateral STEMI: ST-elevation in I, aVL, V5-V6 (LCX territory)
- Posterior STEMI: ST-depression in V1-V3 with tall R-waves (mirror image)
Step 1 Integration: The ECG lead locations correspond to the anatomical position of the heart and coronary territories. Lead placement follows Einthoven’s triangle principles, with each lead representing a different electrical vector. Understanding coronary anatomy helps predict which leads will show changes based on the occluded vessel.
Risk Stratification: From Molecular Markers to Clinical Outcomes
TIMI and GRACE Risk Scores
Risk stratification in ACS helps guide management intensity. The TIMI risk score incorporates clinical variables (age ≥65, ≥3 CAD risk factors, known CAD, aspirin use in past 7 days, severe angina, ST-changes, elevated biomarkers) to predict outcomes.
Step 1 Integration: Advanced age increases risk partly due to decreased cardiovascular reserve and increased comorbidities. The aging heart develops increased collagen deposition, decreased compliance, and reduced β-adrenergic responsiveness, making it less able to compensate for acute ischemia.
Biomarker Integration Beyond Troponin
Additional biomarkers provide prognostic information:
- BNP/NT-proBNP: Indicates heart failure and increased mortality risk
- CRP: Reflects inflammatory burden and plaque instability
- Creatinine: Kidney function affects contrast nephropathy risk and medication dosing
Step 1 Integration: BNP is released from ventricular myocytes in response to wall stretch (preload). It activates guanylyl cyclase, increasing cGMP levels, which causes vasodilation and natriuresis. Elevated BNP in ACS indicates ventricular dysfunction and higher mortality risk.
Pharmacological Management of acute coronary syndromes
Antiplatelet Therapy
Dual antiplatelet therapy forms the cornerstone of ACS management:
Aspirin irreversibly inhibits COX-1, blocking thromboxane A2 production and reducing platelet aggregation.
Step 1 Integration: Aspirin acetylates Ser530 in COX-1, permanently blocking the enzyme. Since platelets lack nuclei, they cannot synthesize new COX-1, making the inhibition irreversible for the platelet’s lifespan (7-10 days). This explains why aspirin’s antiplatelet effect lasts much longer than its analgesic effect.
P2Y12 inhibitors (clopidogrel, prasugrel, ticagrelor) block ADP-mediated platelet activation through different mechanisms.
Step 1 Integration: ADP binding to P2Y12 receptors activates Gi proteins, reducing cAMP levels and promoting platelet activation. Clopidogrel and prasugrel are prodrugs requiring CYP2C19 metabolism for activation, while ticagrelor is a direct, reversible P2Y12 antagonist.
Anticoagulation
Anticoagulant therapy prevents thrombin generation and fibrin formation:
- Heparin activates antithrombin III, inhibiting factors IIa and Xa
- Enoxaparin (LMWH) has more predictable pharmacokinetics
- Bivalirudin directly inhibits thrombin
Step 1 Integration: Heparin’s anticoagulant effect depends on antithrombin III binding, which induces a conformational change that accelerates factor Xa and IIa inhibition by 1000-fold. LMWH has a higher anti-Xa:anti-IIa ratio compared to unfractionated heparin due to shorter chain length.
Beta-Blockers and ACE Inhibitors
Beta-blockers reduce myocardial oxygen demand by decreasing heart rate, contractility, and blood pressure.
Step 1 Integration: Beta-1 receptor blockade prevents cAMP-mediated calcium channel phosphorylation, reducing calcium influx and myocardial contractility. This decreases oxygen consumption (MVO2 = HR × SBP × contractility) and can prevent ischemia extension.
ACE inhibitors provide cardiovascular protection through multiple mechanisms.
Step 1 Integration: ACE inhibition blocks angiotensin II formation and increases bradykinin levels. Angiotensin II normally causes vasoconstriction, aldosterone release, and sympathetic activation. Bradykinin accumulation (normally degraded by ACE) contributes to vasodilation and the characteristic dry cough side effect.
Interventional Management: Timing and Strategy
Primary PCI vs. Fibrinolysis
For STEMI patients, primary PCI is preferred when available within 120 minutes of first medical contact. When PCI isn’t immediately available, fibrinolytic therapy should be considered if no contraindications exist.
Step 1 Integration: Fibrinolytic agents (tPA, reteplase, tenecteplase) convert plasminogen to plasmin, which cleaves fibrin into soluble fragments. The “golden hour” concept reflects the time-dependent salvage of viable but ischemic myocardium before irreversible necrosis occurs.
NSTEMI/UA Management Strategy
NSTEMI and UA patients benefit from early invasive strategy (catheterization within 24 hours) if they have high-risk features: elevated troponin, ST-changes, TIMI score ≥3, or hemodynamic instability.
Complications and Long-term Management
Mechanical Complications
Post-MI mechanical complications include papillary muscle rupture, ventricular septal defect, and free wall rupture. These typically occur 3-7 days post-infarction when necrotic tissue is weakest.
Step 1 Integration: Myocardial healing progresses through inflammation (0-3 days), proliferation (3-14 days), and remodeling (weeks to months). Mechanical complications occur during the proliferation phase when inflammatory cells digest necrotic tissue before collagen deposition strengthens the infarct zone.
Electrical Complications
Arrhythmias are common post-ACS, ranging from benign atrial fibrillation to life-threatening ventricular tachycardia/fibrillation.
Step 1 Integration: Ischemic myocardium develops altered membrane potentials due to ATP depletion and ionic pump dysfunction. This creates areas of delayed conduction and abnormal automaticity, predisposing to reentrant arrhythmias and ectopic activity.
Clinical Pearls for Step 2 Success
- Always consider ACS in chest pain patients, even with atypical presentations
- Serial troponins and ECGs are essential for diagnosis and risk stratification
- Time is muscle: Early recognition and treatment improve outcomes
- Risk stratification guides therapy intensity: High-risk patients need early invasive management
- Medication contraindications matter: Consider bleeding risk, renal function, and drug interactions
Conclusion
Mastering acute coronary syndromes requires integrating pathophysiology, pharmacology, and clinical management principles. By understanding the molecular mechanisms underlying ACS presentation, diagnosis, and treatment, you’ll be prepared for questions across all USMLE steps and clinical rotations. Remember that the new Step 2 format emphasizes this integration—connecting basic science knowledge to clinical decision-making is key to exam success and excellent patient care.
The systematic approach outlined here will serve you well whether you’re answering questions about troponin kinetics on Step 1 or managing a STEMI patient during your cardiology rotation. Focus on understanding the “why” behind each diagnostic test and treatment decision, and you’ll find that ACS becomes one of your strongest topics across all medical training phases.
Thanks again for stopping by! Be sure to check out our other blogs or contact us for tutoring today!