Hyperkalemia: ECG Changes & Emergency Management (USMLE)
Why this matters
Hyperkalemia kills the indecisive. The difference between “hmm” and “give calcium now” is a cardiac arrest. This post gives you a rapid, exam‑proof playbook: what to look for, what to push, and what to stop.
Step 1 integration: Raising extracellular K⁺ depolarizes the resting membrane potential (less negative), inactivating fast Na⁺ channels → slowed conduction and arrhythmias. The Nernst equation & the Na⁺/K⁺‑ATPase pump live behind every ECG change you see.
The big picture (fast)
- When to panic: ECG changes (peaked T’s, PR prolongation, QRS widening → sine‑wave), severe K⁺, or symptoms.
- Immediate goal: stabilize myocardium with IV calcium.
- Shift K⁺ intracellularly: insulin + dextrose, high‑dose β‑agonist, bicarbonate (if acidemic).
- Remove K⁺ from body: loop diuretics, potassium binders, dialysis.
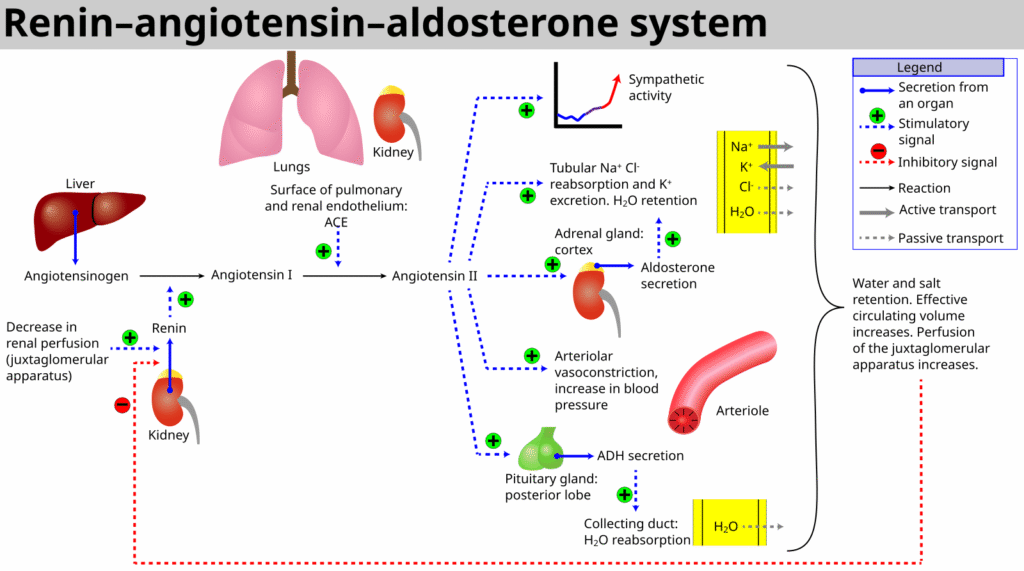
- Stop the cause: meds (ACEi/ARB, spironolactone, trimethoprim, NSAIDs), missed dialysis, tissue breakdown.
- Goal is to avoid cardiac arrest, ACS, and heart failure.
Step 1 integration: Insulin stimulates Na⁺/K⁺‑ATPase → K⁺ influx; β₂‑agonists increase cAMP with similar effect; acidemia shifts H⁺ into cells and K⁺ out via H⁺/K⁺ exchange—fixing pH helps fix K⁺.
Pathophysiology you actually use
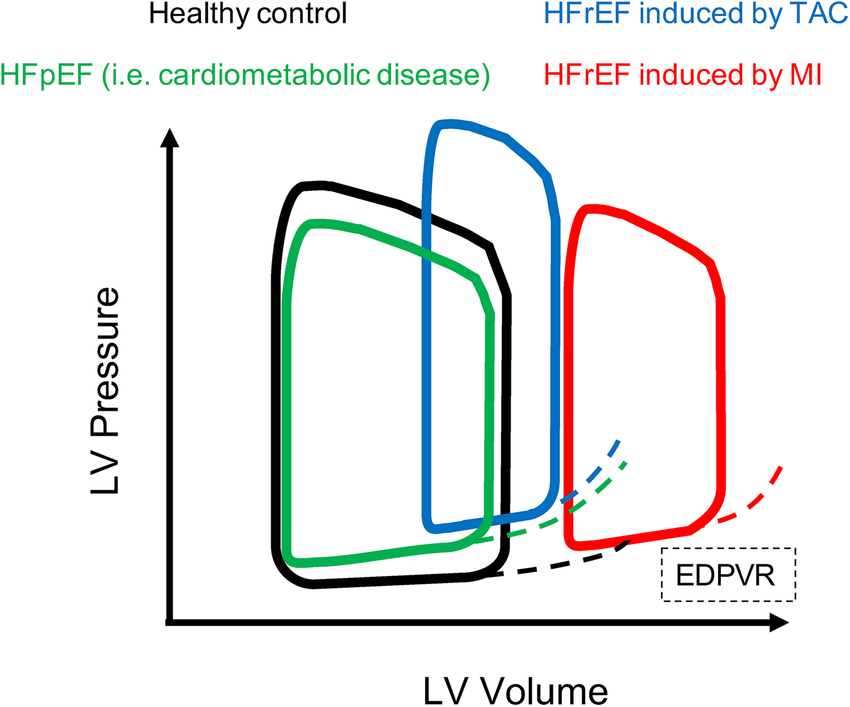
- Renal excretion controls K⁺ long‑term. Aldosterone upregulates ENaC and Na⁺/K⁺‑ATPase in principal cells, favoring K⁺ secretion into the lumen. CKD, hypoaldosteronism, and drugs that block RAAS or ENaC/ROMK crank up serum K⁺.
Step 1 integration: Aldosterone ↓serum K⁺ by ↑ENaC (apical) and ↑Na⁺/K⁺‑ATPase (basolateral). Removal of lumen‑negative potential (e.g., amiloride) reduces K⁺ secretion. - Beware pseudo‑hyperkalemia: hemolyzed sample, prolonged tourniquet, leukocytosis/thrombocytosis. Always re‑draw if the ECG is pristine and the story smells off.
Clinical vignette #1 — DKA trap
A 22‑year‑old with DKA: fruity breath, K⁺ 6.8, bicarbonate 10, glucose 520. ECG shows tall, narrow, peaked T waves in V2–V4.
Moves:
1) Calcium gluconate 1–2 g IV (membrane stabilization).
2) Regular insulin 10 units IV + 25 g dextrose (add D10W if glucose <250 after bolus).
3) High‑dose nebulized albuterol (10–20 mg).
4) Fluids + insulin infusion to fix ketoacidosis (the real problem).
Pearl: Total body K⁺ is low in DKA from osmotic diuresis; serum is “fake high.” Once insulin flows, K⁺ plummets—replace K⁺ when serum K⁺ <5.0 and patient is urinating.
Step 1 integration: Insulin deficiency + acidosis shift K⁺ out of cells; therapy reverses both, driving K⁺ back in and unmasking total body depletion.
Clinical vignette #2 — Dialysis miss + drug stack
A 68‑year‑old with ESRD misses dialysis. Med list: lisinopril + spironolactone + TMP‑SMX. He’s weak; ECG shows PR prolongation, wide QRS. K⁺ 7.2.
Moves now:
1) Calcium chloride 1 g IV via central line (or gluconate peripherally) for immediate stabilization.
2) Insulin + dextrose and albuterol.
3) Call nephrology for urgent hemodialysis (definitive).
4) Hold offending meds.
Step 1 integration: ACEi/ARB ↓aldosterone; spironolactone antagonizes mineralocorticoid receptor; trimethoprim blocks ENaC (amiloride‑like). All three decrease distal K⁺ secretion.
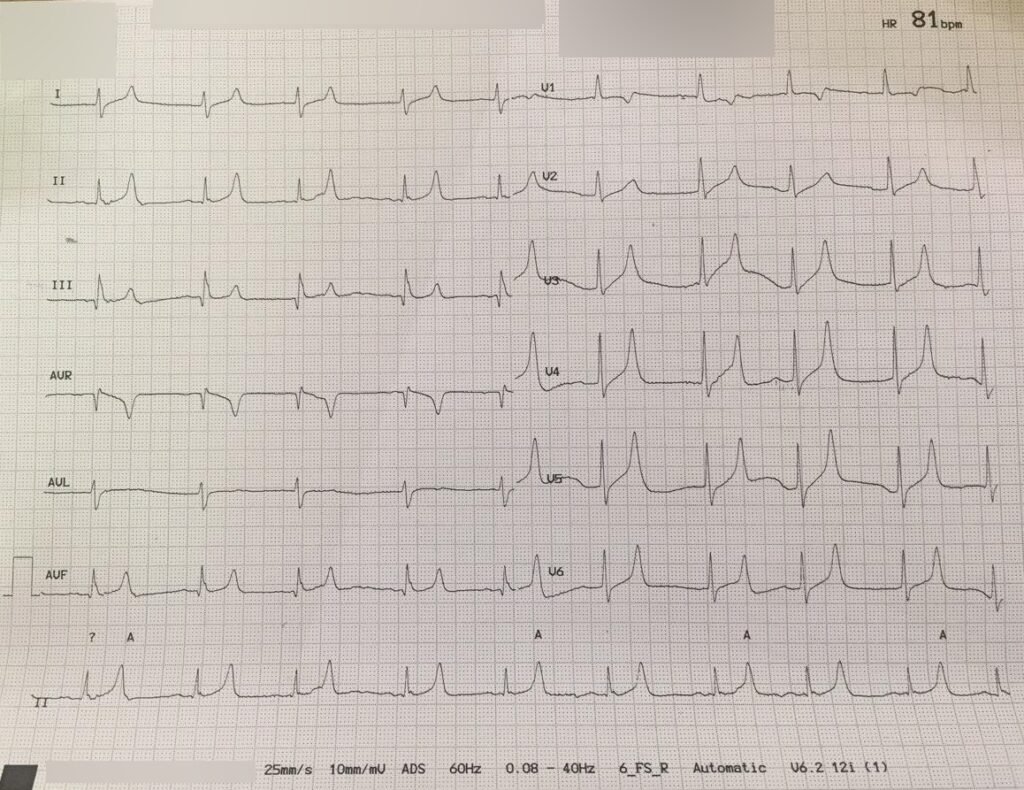
ECG changes: what they actually look like
- Early: narrow, peaked T waves (especially precordial leads).
- Progression: short QT, PR prolongation, QRS widening, loss of P waves, finally sine‑wave and ventricular arrhythmias.
Pro tip: ECG sensitivity is imperfect—treat the patient, not a pretty tracing.
Step 1 integration: Depolarized resting potential inactivates fast Na⁺ channels → slowed phase 0 upstroke → widened QRS; repolarization changes drive T‑wave morphology.
ED/ICU algorithm (simple and safe)
1) Confirm & strip errors: verify non‑hemolyzed sample; get ECG immediately.
2) If ECG changes or K⁺ ≥6.0 or symptomatic:
- Calcium gluconate 1–2 g IV (or calcium chloride 1 g IV, central). Repeat if QRS still wide.
3) Shift K⁺ into cells (temporary): - Regular insulin 10 units IV + 25 g dextrose (skip dextrose if glucose ≥250; re‑check glucose q30–60 min).
- Albuterol 10–20 mg nebulized (or 2–4 mg IV if available).
- Sodium bicarbonate 50–100 mEq IV if pH ≤7.1 or severe metabolic acidosis.
4) Remove K⁺ (definitive): - Loop diuretic + fluids if kidneys work.
- Potassium binders: sodium zirconium cyclosilicate or patiromer (onset hours; SPS is legacy and has GI risks).
- Hemodialysis for ESRD or refractory cases.
5) Stop sources: RAAS blockers, K‑sparing diuretics, NSAIDs, trimethoprim, heparin (hypoaldo), supplements, salt substitutes.
6) Re‑check K⁺ & ECG q1–2h until stable; watch for rebound.
Step 1 integration: Distal nephron K⁺ secretion needs a lumen‑negative potential (Na⁺ uptake via ENaC). Block ENaC (amiloride/trimethoprim) → less negativity → less K⁺ secretion.
Testing extras you might see
- TTKG (trans‑tubular K gradient): in true hyperkalemia, a low TTKG suggests impaired aldosterone effect or distal flow; not needed for emergent care but fair game for exams.
- Magnesium & calcium: correct concomitant abnormalities that worsen arrhythmias.
- Tumor lysis/rhabdo: aggressive fluids, treat underlying cause, consider rasburicase in TLS.
Step 1 integration: Cell lysis and acidosis raise serum K⁺; β₂ agonism and alkalosis lower it by intracellular shift.
Take‑home (tattoo this)
Stabilize with calcium, shift with insulin/β₂/bicarb, remove with diuretics/binders/dialysis, and stop the causes. If the QRS is fat, don’t philosophize—push calcium.
Thanks again for stopping by! Be sure to check out our other blogs or contact us for tutoring today!